Millions of women worldwide grapple with chronic pelvic pain disorders (CPPDs), conditions like endometriosis, uterine fibroids, and pelvic inflammatory disease that inflict persistent pain and discomfort. Beyond the physical burden, these disorders often trigger a cascade of mental health challenges, including anxiety and depression, significantly diminishing their quality of life. However, recent research offers a beacon of hope: exercise.
The Link Between Chronic Pelvic Pain and Mental Health
Chronic pelvic pain (CPP) is defined as pain in the area below the belly button and between the hips that lasts for six months or more. It is often associated with conditions like endometriosis and adenomyosis, although pelvic pain can exist on its own. Studies reveal a strong correlation between CPP and mental health disorders. Women with CPP experience much higher rates of psychological distress compared to those without chronic pain. As many as 80% of women with CPP also have anxiety and depression. Pelvic pain patients are also more likely to experience distressing mental health conditions, such as PTSD and panic disorder. This paints a clear picture: CPP doesn’t just affect the body; it profoundly impacts the mind.
The reasons for this link are multifaceted. The constant pain can lead to feelings of helplessness, frustration, and social isolation, all of which contribute to mood disorders. Furthermore, CPP can interfere with sleep, work, and relationships, exacerbating emotional distress. In addition, there may be shared biological mechanisms that make individuals vulnerable to both chronic pain and psychological disorders. These include genetic, environmental, inflammatory, and neurobiological factors.
Exercise: A Ray of Hope
A groundbreaking study by researchers at the Mount Sinai Health System, published in the Journal of Pain Research, has unveiled the significant positive influence of physical activity on the mental health of women battling CPPDs. The study highlights that regular exercise can lead to measurable improvements in mental well-being, regardless of pain levels or a history of anxiety or depressive disorders.
Key Findings of the Mount Sinai Study
The study tracked 76 women diagnosed with CPPDs over 14 weeks. Participants used a specially designed app to monitor their mental health, physical functioning, and pain levels weekly. Fitbit devices tracked their daily physical activity. Analyzing over 4,200 days’ worth of data, the researchers discovered several key insights:
- Improved Mental Well-being: Activities like brisk walking and aerobic exercise were linked to significant improvements in mental well-being.
- Benefits Independent of Pain Levels: The mental health benefits of exercise were observed regardless of the participants’ pain levels or history of mental health disorders.
- Delayed Gratification: The study’s most striking revelation was the delayed mental health benefits associated with exercise, which seemed to manifest a few days after physical activity.
These findings suggest that exercise should be viewed not just as a treatment for physical symptoms but as a comprehensive therapy supporting overall mental and emotional health.
How Exercise Enhances Mental Well-being
The mechanisms by which exercise improves mental health in women with CPPDs are complex and varied.
- Endorphin Release: Exercise stimulates the release of endorphins, the body’s natural painkillers and mood elevators. These neurochemicals can help reduce pain perception and promote feelings of well-being.
- Stress Reduction: Regular physical activity can help lower stress hormones and reduce muscle tension, leading to a more relaxed state of mind.
- Improved Sleep: Exercise can promote better sleep quality, which is crucial for managing mood and overall mental health.
- Increased Self-Esteem: Achieving exercise goals, even small ones, can boost self-confidence and improve body image.
- Social Interaction: Exercising with others provides opportunities for social connection and support, combating feelings of isolation.
- Distraction from Negative Thoughts: Physical activity can provide a welcome distraction from pain and negative thoughts, allowing for a mental break.
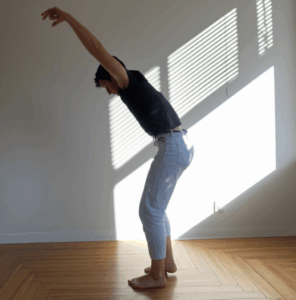
Types of Exercise for Women with Chronic Pelvic Pain
While the benefits of exercise are clear, choosing the right type of physical activity is crucial for women with CPPDs. High-impact exercises can exacerbate pain and discomfort. Instead, focus on low-impact activities that are gentle on the pelvic region:
- Walking: Brisk walking is an accessible and effective way to improve cardiovascular health and mood.
- Swimming: Swimming provides a full-body workout without placing undue stress on the pelvic floor.
- Cycling: Cycling is another low-impact option that can improve cardiovascular fitness and leg strength.
- Yoga: Gentle yoga and stretching can improve flexibility, reduce muscle tension, and promote relaxation. Certain yoga poses can specifically target the pelvic area, providing relief from pain and discomfort. Mindfulness practices associated with yoga also help manage the psychological aspects of chronic pain.
- Pilates: Pilates focuses on core strength and stability, often incorporating modifications that are gentle on the pelvic floor.
- Pelvic Floor Exercises: Strengthening and relaxing pelvic floor muscles through exercises such as Kegels can alleviate pain and improve function, and targeted exercises can help manage symptoms effectively.
- Stretching: A pelvic floor physiotherapist can recommend different exercises to help you relax and coordinate your pelvic floor muscles, and gentle stretches for your stomach and muscles on the outside of your pelvis. These exercises can also reduce pain and may improve bladder, bowel and sexual function.
It is crucial to work with a healthcare professional or physical therapist to develop a tailored exercise plan that considers individual needs and limitations.
Additional Strategies for Managing Chronic Pelvic Pain and Promoting Mental Well-being
In addition to exercise, several other strategies can help women manage CPP and improve their mental health:
- Pain Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and muscle relaxants can help alleviate pain.
- Hormone Treatment: Hormone treatment can help with pain associated with menstruation.
- Pelvic Floor Physical Therapy: Physical therapy can alleviate muscle pain. A pelvic floor physiotherapist can recommend exercises to help relax and coordinate pelvic floor muscles.
- Counseling: Talking to a mental health professional can help develop coping methods for pain, depression, sexual problems, and relationship issues.
- Mindfulness and Meditation: These practices can help manage stress and reduce pain perception.
- Lifestyle Changes: Diet improvements and better posture may offer relief. An anti-inflammatory diet, rich in fruits, vegetables, whole grains, and healthy fats, can reduce inflammation and pain.
- Adequate Sleep: Poor sleep quality can exacerbate pain and mental health issues.
- Stress Management: Chronic stress exacerbates pain perception and can lead to muscle tension and inflammation. Techniques such as mindfulness, meditation, and deep-breathing exercises are effective in managing stress and reducing pain.
A Holistic Approach to Healing
Chronic pelvic pain is a complex condition that requires a holistic approach to treatment. By integrating exercise with other therapies and lifestyle modifications, women can effectively manage their pain, improve their mental well-being, and reclaim their lives. As research continues to illuminate the benefits of physical activity, it is crucial for healthcare systems and patients alike to prioritize exercise as a viable and sustainable path toward improving the quality of life for individuals suffering from chronic pelvic pain.